Macular Degeneration
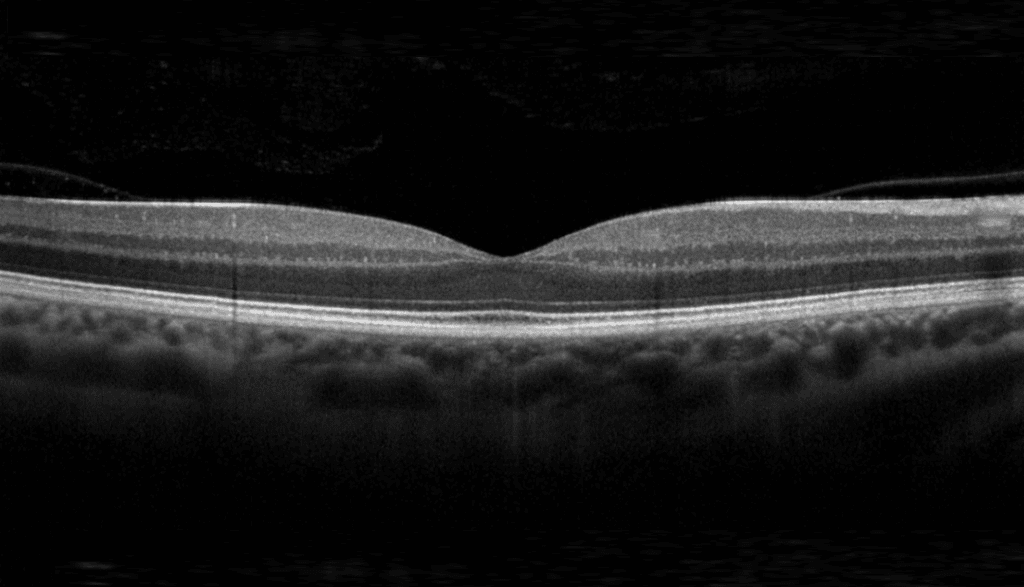
There are two types of macular degeneration. Most people (about 75%) have a form called “early” or “dry” macular degeneration, which develops when there is a build-up of waste material under the macula and thinning of the retina at the macula. Most people with this condition have near normal vision or milder sight loss.
A minority of patients with early (dry) macular degeneration can progress to the vision-threatening forms of macular degeneration called late macular degeneration.
The commonest form of late macular degeneration is “exudative” or “wet” macular degeneration. Wet macular degeneration occurs when abnormal blood vessels grow underneath the retina. These unhealthy vessels leak blood and fluid, which can prevent the retina from working properly. Eventually the bleeding and scarring can lead to severe permanent loss of central vision, but the eye is not usually at risk of losing all vision (going 'blind') as the ability to see in the periphery remains. There is a rarer form of late macular degeneration called geographic atrophy, where vision is lost through severe thinning or even loss of the macula tissue without any leaking blood vessels.
Young patients can develop a similar problem (a choroidal neovascular membrane or CNVM) due to inflammation, trauma or myopia. The treatment for these is slightly different to age related macular degeneration, but also involved injecting medication into the eye to improve vision
Retinal Vein Occlusion
Occlusion (blockage) of a retinal vein is a common cause of sudden painless reduction in vision in older people.
The retina is the thin membrane that lines the inner surface of the back of your eye. Its function is similar to that of the film in a camera. Blockage of one of the veins draining blood out of the eye causes blood and other fluids to leak into the retina, causing bruising and swelling as well as lack of oxygen. This interferes with the light receptor cells and reduces vision.
The condition is uncommon under the age of 60 but becomes more frequent in later life.
There are two types of retinal vein occlusion:
Branch retinal vein occlusions are due to blockage of one of the four retinal veins, each of which drains about a quarter of the retina
Central retinal vein occlusion is due to blockage of the main retinal vein, which drains blood from the whole retina
In general, visual loss is more severe if the central retinal vein is blocked.
Blockages of blood vessels can also occur in uveitis. Sometimes, the main arteries or veins can get blocked, however, often, it’s the tiny capillaries that become obstructed due to inflammation. Treatment is often a complied approach of anti inflammatory medication and laser.
Diabetic Retinopathy
Many diabetics – particularly those with poor diabetic control have damaged blood vessels in the retina, the tissue lining the back of the eye that detects light and allows us to see. This condition, called diabetic retinopathy, affects up to eight out of 10 patients who have had diabetes for 10 years or more.
Many people with mild diabetic retinopathy have good vision, but there are two types of sight-threatening diabetic retinopathy: diabetic macular oedema (DMO) and proliferative diabetic retinopathy (PDR).
In DMO, fluid leaks out of the tiny damaged blood vessels in the back of the eye, and accumulates in the macula, the central part of the retina which is responsible for seeing fine details and central vision. This leads to swelling of the tissue and blurred vision. Eventually, patients with diabetic macular oedema can develop poor central vision and be unable to read or drive, but the vision to the side usually remains normal.
Proliferative diabetic retinopathy is when the retinal blood vessels close resulting in the retina being starved of blood. This causes abnormal and very fragile blood vessels to grow on the surface of the retina which can lead to permanent loss of vision from bleeding into the eye, retinal scarring and retinal detachment.